Ankylosing spondylitis is likely a term that you haven’t heard before unless you’ve been diagnosed with the condition. It’s a condition that affects roughly 1 in 20 adults. There are a wide variety of common symptoms that may be mistaken for signs of other conditions and preventing you from receiving the proper care that you need. But what is Ankylosing spondylitis? This short guide will explore that as well as what triggers it and the best treatment options for this condition.
What exactly is Ankylosing spondylitis?
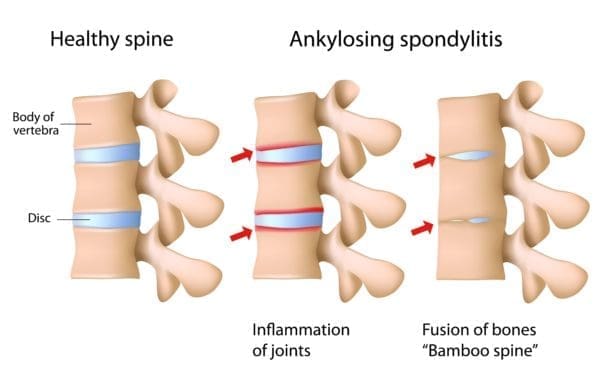
Ankylosing spondylitis is a type of arthritis that typically affects the back and spine. Ankylosis refers to an abnormal loss of mobility and stiffening of the joints as a result of bones fusing together. Spondylitis is the inflammation of the joints of the spine and backbone.
People with Ankylosing spondylitis suffer from joints and ligaments pain. They become stiff and inflamed. Oftentimes, bones within the spine may fuse together resulting in a loss of flexibility. It’s also possible for other joints such as the shoulders, knees, hips and ankles also to be affected.
How serious is Ankylosing spondylitis?
Ankylosing spondylitis is not typically associated with a higher mortality rate compared to a healthy population sample. However, there is a strong correlation between those with the condition and an increased risk of heart attack by 35% and a risk of dying from a stroke by 60% if left untreated.
Generally, symptoms of Ankylosing spondylitis involve moderate to severe pain including redness, swelling and discomfort in the spine or along the bones in the lower back. Symptoms vary on a case-by-case basis. Some people simply experience a periodic mild back pain while others may have severe, chronic pain.
In the most advanced cases, increased swelling leads to the fusion of two or more bones along the spine which can create respiratory problems. Ankylosing spondylitis may sometimes affect other parts of your body including your respiratory and digestive systems. If you are suffering from other health issues, be sure to notify your doctor as they may be related.
Who does Ankylosing spondylitis most commonly affect?
Ankylosing spondylitis most commonly develops in adolescence or early adulthood. Men are twice as likely as women to develop the condition. Family history is one of the most significant determining factors as the gene is passed down hereditarily.
Doctors typically diagnose the condition via blood tests along with x-rays and other imaging tests. A physical test can also determine and demonstrate common symptoms such as a lack of joint mobility.

What are the treatment options?
Unfortunately, there is no cure for Ankylosing spondylitis. There are many effective treatment options that stall the progression of the disease and manage symptoms though. Your doctor will likely recommend some combination of the diet, exercise, and medicine. In more serious cases, surgery may be necessary to repair joints.
Exercise
For those with a family history of Ankylosing spondylitis even if it hasn’t been diagnosed, exercise is an essential way to prevent/mitigate the onset of the early stages of the disease. The goal should be to focus on exercises that increase your flexibility and muscle strength. If you already suffer from the condition, be sure to consult with your doctor to help determine the best exercise regimen for you. It may be necessary for you to begin a physical therapy program first to help build your strength and flexibility initially.
Aerobic and deep breathing exercises are a great way to help keep your chest and rib cage flexible. In addition, swimming is an excellent choice as it is low impact but promote overall flexibility of your spine along with neck, shoulder and arm movement along with breathing.
Check out simple exercises for Ankylosing spondylitis below:
Diet
A healthy diet is essential for everyone. For those with Ankylosing spondylitis, research is starting to show the benefit. You want a diet that promotes bone health. Research is still in its early stages but foods high in omega-3 fatty acids such as avocados, kale and walnut can be beneficial in fighting inflammation and improving joint health.
Learn more which foods to avoid and which foods incorporate into your diet here.
Medication
There are a wide of medicine used to treat Ankylosing spondylitis. Once again, it’s essential to talk to your doctor
And discuss things like medical history, pain and stiffness, your lifestyle and so on to find the best medicine for you. Similar to treating arthritis, the most common choices are the following:
- Nonsteroidal anti-inflammatory drugs (NSAIDS): These medications reduce pain and swelling and include familiar names like ibuprofen, aspirin, naproxen and so on. The added bonus is some of these also promote heart health.
- Corticosteroids: These medications are much stronger and can work to fight intense pain and joint stiffness. Do note though that they are not usually the best long-term treatment option as they have other side effects.
- Biologic agents: This newer class of medicine is still in its early stages but has been found effective in blocking the proteins associated with Ankylosing spondylitis symptoms.
- Disease-modifying anti-rheumatic drugs: These drugs are specifically designed to treat arthritis and Ankylosing spondylitis and are often used in combination with NSAIDs to help reduce to the total overall amount of medication a patient needs to take.
Surgery
Surgery is typically reserved for the most advanced and painful cases of Ankylosing spondylitis often when medication is not enough to overcome the chronic pain. Most often, joint replacement particularly in the knees and hips or in rare cases, surgeries to strengthen the spine.

The bottom line
Ankylosing spondylitis is a serious condition, but it is one that you can manage. If you’re open and honest with your doctor, see her regularly, exercise consistently, have good posture and maintain a good diet, you can manage a healthy and active life and not be held back from doing the things you want to do.
How do you manage Ankylosing spondylitis?
Tell us about your experience in the comments below.
What topics related to living with Ankylosing spondylitis would you like to see us explore?
Email us at info@painresource.com with your ideas!
Are you on Facebook?
Join our online community by clicking here.
This post was updated in January 2019 with new information and resources.





My grandad was in a dump truck roll over years ago. He was always severely bent over and had a hard time breathing. I don’t know if he had AS but it sure looked like it. I have the HLA B27 marker and severe spinal problems.I had a severe spinal injury in 1978 and deal with lots of pain now. I had adequate pain relief from 1997 until 2017 when the CDC listed prescribing guidelines for opioids. Now I’m back to suffering quite a bit. My scrailiac is one of my biggest problems with pain.
I constantly read that to exercise and have found out for years it causes more pain than helps. It causes enough pain that I can’t get any sleep. I use NSAIDs from time to time but I’m not suppose to because of heart issues. I am on a small dosage of morphine that helps immensely but my pain doctor is not willing to raise the dosage. I had taken a larger dose of methadone for 20 years until the CDC lied about their prescribing guidelines and doctors ran for the hills and quit pain management. Hopefully doctors will get together and get back to doctoring without the DEA or CDC interferring.