As of right now, the demand for the vaccine is much greater than the supply of vaccine doses. This means that in most states, there is a priority list to determine who is able to have the COVID vaccine first. So, where does this leave people with chronic pain in the midst of the pandemic? Should people with chronic pain be prioritized when the COVID vaccine is distributed? Unfortunately, the answer is not as simple as you might think.
Information on the COVID-19 Vaccination Process
 First, we must understand that there are simply not enough vaccine doses available to every single person in the United States—and throughout the world—who needs protection against COVID-19. Currently, there are two main distributors of the vaccine in the United States that have been approved for emergency use only by the Food and Drug Administration (FDA): the Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine. The Pfizer-BioNTech vaccine is recommended for people aged 16 and older while the Moderna vaccine requires you to be at least 18 years old.
First, we must understand that there are simply not enough vaccine doses available to every single person in the United States—and throughout the world—who needs protection against COVID-19. Currently, there are two main distributors of the vaccine in the United States that have been approved for emergency use only by the Food and Drug Administration (FDA): the Pfizer-BioNTech COVID-19 vaccine and the Moderna COVID-19 vaccine. The Pfizer-BioNTech vaccine is recommended for people aged 16 and older while the Moderna vaccine requires you to be at least 18 years old.
Both of these are mRNA vaccines, which are specifically made to help the cells in our bodies go through the process of triggering immune responses that create antibodies to fight against any future exposure to the virus. The Pfizer-BioNTech and Moderna COVID-19 vaccines each require two doses, spaced apart by at least three weeks, for optimal protection.
The Centers for Disease Control and Prevention (CDC) released recommendations on who should get first access to the COVID vaccine. The CDC has previously separated priority groups into three categories (1a, 1b, and 1c). Each phase of distribution, they recommended, should offer vaccines to the groups sequentially before opening up vaccine availability to other populations.
 However, the CDC recently expanded vaccine priority to people who are 65 years or older as well as adults who have underlying medical conditions in order to encourage more people to be vaccinated. In addition to these new guidelines, the most up-to-date priority groups are as follows:
However, the CDC recently expanded vaccine priority to people who are 65 years or older as well as adults who have underlying medical conditions in order to encourage more people to be vaccinated. In addition to these new guidelines, the most up-to-date priority groups are as follows:
- 1a— Healthcare workers, including nurses, doctors, and long-term caretakers should have immediate access to the vaccine, according to the CDC, as they are most likely to be exposed to the virus through their profession. This also includes people in long-term care facilities, such as nursing homes.
- 1b— The next priority group covers a large amount of frontline or essential workers. This includes firefighters, police officers, Postal Service employees, teachers, and public transit workers.
- 1c— The third group who needs the vaccine in this first wave of distribution includes other essential workers who have frequent contact with the public, such as food service workers and people in the public health field.
It’s important to note, though, that each individual state is ultimately able to decide how they approach their own vaccine distribution. Even if you are 65 or older, have an underlying health condition, or fall into one of these three categories of occupations, you will have to check with your state’s guidelines to know if you are eligible to be vaccinated.
Are People with Chronic Pain Considered High Risk for COVID-19?
 The variability in state access (and guidelines) for the COVID vaccine leads us to the big question: Are people who have chronic pain in one of these three priority groups? The truth is that there are many different factors that go into determining your own eligibility for the vaccine.
The variability in state access (and guidelines) for the COVID vaccine leads us to the big question: Are people who have chronic pain in one of these three priority groups? The truth is that there are many different factors that go into determining your own eligibility for the vaccine.
First, of course, is your occupation. As you can see outlined in the three groups described above, certain professions are prioritized over others. If you experience chronic pain and you happen to be a nurse, your chances of having access to the vaccine are probably much greater than those of someone who works from home and has chronic pain.
However, your own risk for COVID-19 plays a role in your vaccine eligibility as well. Not only do you have to assess your risk of exposure, but you have to evaluate if you are more susceptible to the virus’ effects. But chronic pain does not always equate to being high risk, just as you might be high risk without having chronic pain.
There are countless reasons as to why somebody might have chronic pain. For reference, chronic pain is persistent, long-lasting, and typically incurable. Chronic pain might be in one centralized location for some people, but it can also be systemic for others, meaning that it is not focused to just one area of the body.
Chronic pain typically presents with physical symptoms, though it also often causes emotional challenges as a result of social isolation, especially during the pandemic. Additionally, chronic pain can lead to other challenges that do lower your immune system’s response to illness, such as depression and substance abuse.
The onset of chronic pain can come from a variety of ailments—anything from injury, surgery, illness, genetic disorders, autoimmune diseases, and much more can cause chronic pain. In some cases, whatever is causing the chronic pain can also increase your chances of falling dangerously ill from COVID-19. Thus, you must work with your health care providers and trusted support system to understand if you have chronic pain and simultaneously are at high risk.
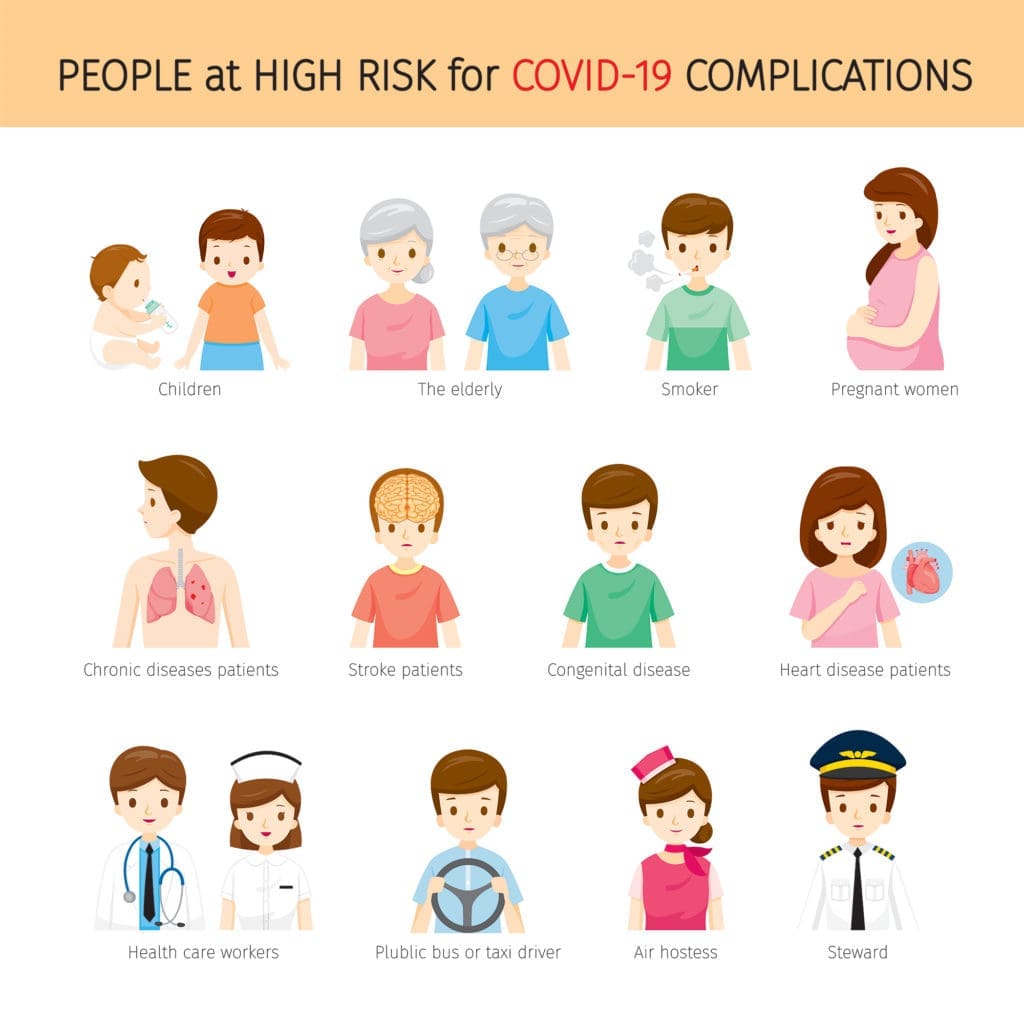
People who are generally considered high risk include (but are not limited to) those who have:
- Cancer
- Down syndrome
- Lung disorders
- Autoimmune disorders
- Heart disease
- Weakened immune system
Depending on your health symptoms, occupation, and susceptibility to the virus, you might be next in line to receive the COVID vaccine. If you do have underlying medical conditions and/or chronic pain, always be sure to speak with your doctor to make sure that you are a good candidate for the vaccine before making any decisions.
The Next Steps
 For people with chronic pain—and even those without—who are ready to get the COVID vaccine, the next steps are to check with your healthcare providers to confirm that any medical conditions you may have will not interact with the effectiveness of the vaccine. Vaccine safety is essential to preventing COVID-19 as well as any serious side effects, like an allergic reaction.
For people with chronic pain—and even those without—who are ready to get the COVID vaccine, the next steps are to check with your healthcare providers to confirm that any medical conditions you may have will not interact with the effectiveness of the vaccine. Vaccine safety is essential to preventing COVID-19 as well as any serious side effects, like an allergic reaction.
Moreover, preventing COVID-19 will take more than a safe and effective vaccine. Even after you receive your vaccination, the U.S. Department of Health and Human Services emphasizes the importance of continuing the same safety protocols as before. This means that you will still need to wear a mask, practice social distancing guidelines, and limit the spread of illness through good hygiene.
It may seem as though there is no end in sight to this pandemic, but with the COVID vaccine working to protect those who are at the highest risk of infection, we continue to move forward toward a safer world.
What questions do you have about COVID vaccinations?
Tell us in the comments section below!


I recently read an article that the researchers had studied covid and chronic illness, like autoimmune disease-RA or cancer etc. It stated if you are taking DMARDS or immunosuppressants it’s pointless to get the vaccine. Your body’s immune response is purposely being suppressed so you are not able to make antibodies anyway? Makes sense to me but I wonder if anyone has had the experience with having chronic illness and has gotten the vaccine and it wasn’t effective.
i have fibromyalgia and osteoarthritis, i also have a down syndrome daughter who has asthma and moya-moya, factor x clotting disorder and a history of dvt’s. I need to know if this vaccine is going to be safe enough for us to get.