Your colon is an extremely important organ in your body. It helps extract nutrients from undigested food and eliminates waste products through the rectum as feces. When the large intestine becomes inflamed, it is known broadly as colitis. This inflammation can cause severe symptoms such as diarrhea, bloody stool, and abdominal pain. One of the main causes of this inflammation is a condition called ulcerative colitis. But, what is ulcerative colitis, and how can you tell if you have it? Below, we’ll cover everything you need to know about this common, chronic condition. First, let’s start by examining what ulcerative colitis is in the first place.
What Is Ulcerative Colitis?
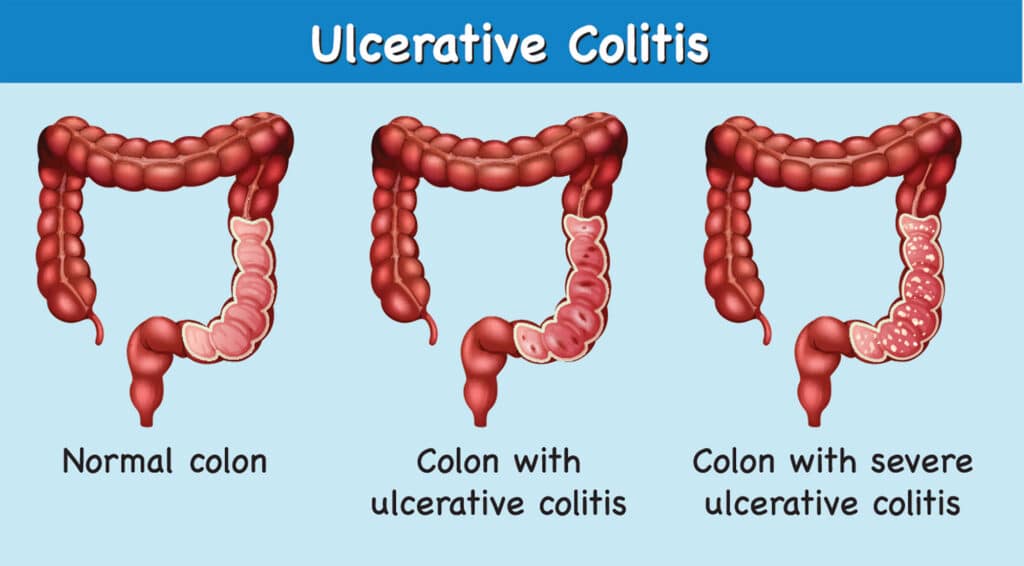 Ulcerative colitis (UC) is a chronic disease of the large intestine that causes the lining of the colon to become inflamed and develop tiny open sores, or ulcers. UC is a type of inflammatory bowel disease (IBD), which are a group of diseases that affect the gastrointestinal (GI) tract.
Ulcerative colitis (UC) is a chronic disease of the large intestine that causes the lining of the colon to become inflamed and develop tiny open sores, or ulcers. UC is a type of inflammatory bowel disease (IBD), which are a group of diseases that affect the gastrointestinal (GI) tract.
The inflammation caused by UC causes your bowel to move its contents rapidly and empty frequently. As cells on the surface of the lining of your bowel die, ulcers form. The ulcers may cause bleeding and discharge of mucus and pus. This inflammation typically begins in the rectum and spreads upwards. In some cases, UC can involve your entire colon.
UC is a fairly common condition. Together with Crohn’s disease, another type of IBD, it affects up to 1 in 250 people in North America and Europe. UC can affect anyone, at any age. However, most people develop the condition between the ages of 15 and 30 years old, according to the American Gastrointestinal Association (AGA).
There are additional risk factors for UC, which include having a close relative with UC or IBD, being a male over the age of 50, and frequent use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil® or Motrin®). Additionally, there appears to be a higher prevalence of UC among Jewish individuals, although the reason why is still unclear.
UC can cause a host of unpleasant symptoms, which we will take a look at next.
Symptoms of Ulcerative Colitis
Symptoms of UC van vary depending on the severity of your condition, age, what area of your GI tract is affected, and several other factors. Your symptoms may also change over time due to many factors such as lifestyle changes and treatments.
People diagnosed with UC can experience symptoms that range from very mild to severe. They may also experience no symptoms at all, which can be caused by UC going into remission. However, symptoms can return, and when they do they can become severe. This type of coming and going is known as a flare-up and is common for many chronic conditions that affect the GI tract.
Common symptoms of UC may include:
- Bloody stools
- Abdominal pain
- Diarrhea
- Rectal pain
- Unintended weight loss
- Malnutrition
- Abnormal or increased abdominal sounds
UC can also cause symptoms that may not be typically associated with GI issues or IBD-related conditions. These may include:
- Joint pain
- Nausea and vomiting
- Skin problems
- Eye inflammation
- Mouth sores
What Causes Ulcerative Colitis?
According to the Crohn’s and Colitis Foundation, UC is thought to be the result of several factors, including an abnormal immune system response, although these factors are not yet well understood. Other theories as to the cause of UC include genetics, microbiome, and environmental factors such as viruses or bacteria.
Research suggests that UC could be triggered by an interaction between a virus or bacterial infection in the colon, which could cause the immune system to attack healthy cells. Typically, the cells and proteins that make up your immune system protect you from infection. In a normal immune response, the immune system would cause temporary inflammation that would subside once the infection or illness has left the body.
In UC patients, the inflammation persists long after the immune system should have finished its job. In this instance, the body continues to send white blood cells into the lining of the large intestine, which can produce chronic inflammation and ulcers.
Types of Ulcerative Colitis
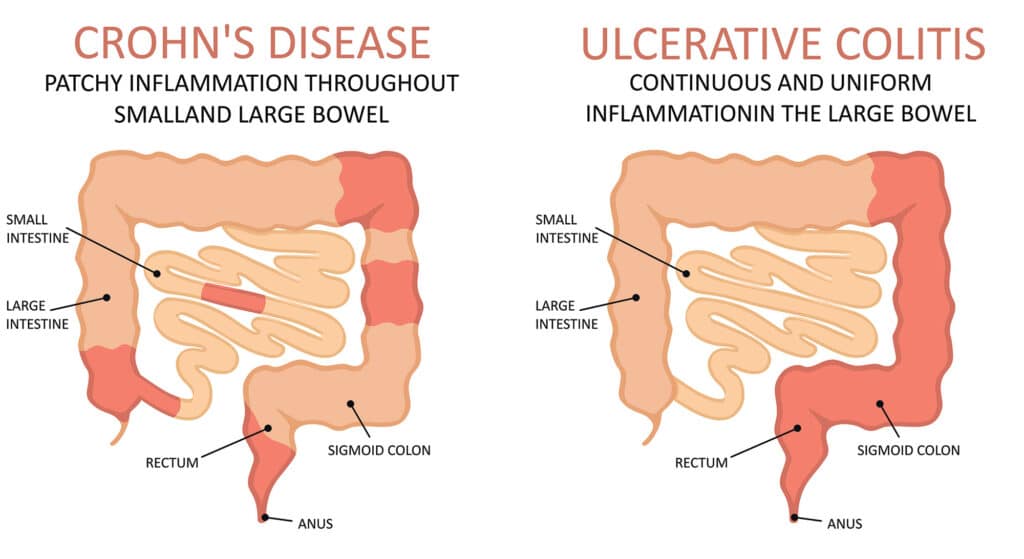
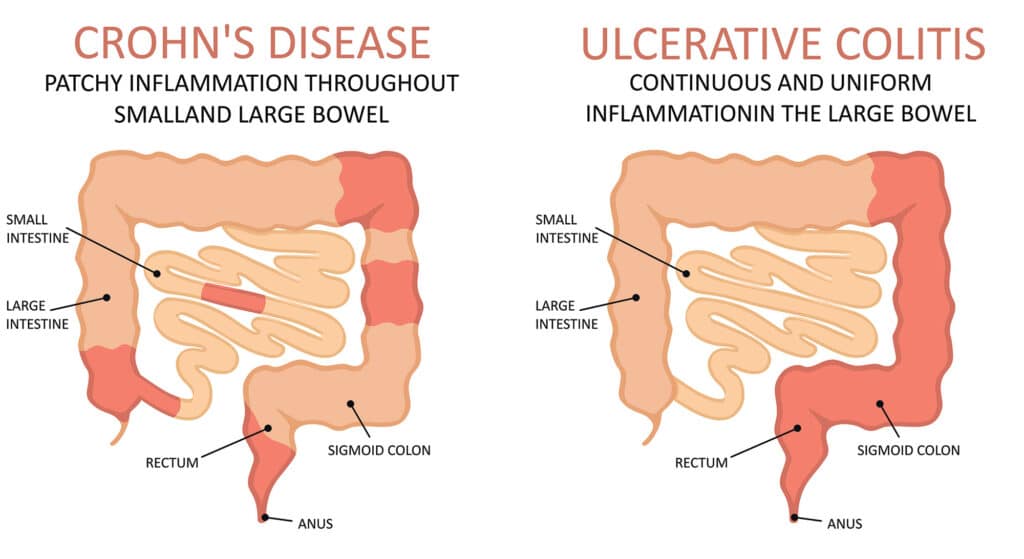
- Ulcerative proctitis: This type of UC is classified as inflammation that is confined to the area closest to the anus (rectum), which typically causes rectal bleeding. This is oftentimes the only symptom of ulcerative proctitis.
- Proctosigmoiditis: Inflammation that involves the rectum and sigmoid colon (the lower end of the colon) is known as proctosigmoiditis. Symptoms of proctosigmoiditis include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Left-sided colitis: When inflammation extends beyond the sigmoid colon and descending colon, it is classified as left-sided colitis. Signs and symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and urgency to defecate.
- Pancolitis: This type often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
Getting a Diagnosis
If you notice that you are displaying symptoms of UC, or if you believe you may be at risk, it may be time to talk with your doctor. See your doctor if you experience a persistent change in your bowel habits or if you have signs and symptoms such as:
- Severe abdominal pain
- Blood in your stool
- Diarrhea that awakens you from sleep
- Unexplained fever
If your doctor suspects you may have UC, they may proceed with tests that can help get you a proper diagnosis.
Tests that can help diagnose or rule out UC include:
- Blood tests: Blood tests are often one of the first types of tests your doctor will recommend. They are often useful in the process of diagnosing UC. A complete blood count (CBC) looks for signs of anemia (a low red blood cell count). Other blood tests can help indicate inflammation such as a high level of C-reactive protein and a high sedimentation rate.
- CT scan: A CT scan is a specialized X-ray of your abdomen and pelvis. This is typically used if your doctor suspects a complication from UC. A CT scan may also reveal how much of the colon is inflamed.
- Stool test: White blood cells or certain proteins in your stool can indicate UC. A stool sample can also help rule out other disorders, such as infections caused by bacteria, viruses, and parasites.
- Biopsy: While not always necessary or common, your doctor may recommend a biopsy to help determine or rule out UC. A biopsy is a process in which a surgeon removes a tissue sample from your colon for analysis.
- Colonoscopy: During a colonoscopy, your doctor inserts a lighted scope known as a colonoscopy into your rectum to examine the inside of your colon.
What Does Treatment Look Like?
Treatment for UC typically involves either drug therapy or surgery. The primary goal of any UC treatment is to help patients regulate their immune systems better. While there is no known cure, a combination of treatment options can help you live a more rewarding life, with fewer symptoms and more control over your condition.
Medications
Depending on what type of UC you have, how severe your symptoms are, and what your doctor feels is best for you, the type of medication you’ll take can vary.
For more mild symptoms, your doctor may prescribe medications to reduce inflammation and swelling. This is often the first course of treatment and will help alleviate many of your symptoms. These types of medications can include:
- Mesalamine (Asacol HD, Lialda)
- Sulfasalazine (Azulfidine)
- Balsalazide (Colazal)
- Olsalazine (Dipentum)
For more severe symptoms, your doctor may prescribe a type of medication known as a biologic. Biologics are a drug made of antibodies that are designed to help reduce and stop inflammation. These drugs can help your UC go into remission, and can reduce flare-ups. They include, but are not limited to, the following:
- adalimumab (Humira)
- golimumab (Simponi)
- infliximab (Remicade)
- tofacitinib (Xeljanz)
Should medications fail to help, your doctor may recommend surgery.
Surgery
Surgery is not always necessary for UC. However, if you experience severe symptoms such as substantial blood loss, debilitating symptoms, severe blockage, or a perforation of your colon, surgery may be necessary.
Surgery for UC typically involves removing your entire colon and rectum as well as creating a new pathway for waste. This pathway can be out through a small opening in your abdominal wall. To redirect waste through your abdominal wall, the surgeon will make a small opening where they will then connect the end of your small intestine to. Waste will drain through the opening and into a bag, known as an ostomy bag.
Other surgical procedures involve removing specific damaged or diseased parts of the colon, while still retaining the outer muscles of your rectum. In this instance, the surgeon attaches your small intestine to the rectum to form a small pouch. This procedure still allows you to pass stool through your rectum, however, bowel movements will become more frequent and watery than normal.
Have More Questions? Still Wondering, “What Is Ulcerative Colitis?”
Ask us your questions in the comments section below!
What topics related to ulcerative colitis should we cover next?
Email us your ideas at info@painresource.com, we may just feature yours in a future article!
Are you living with ulcerative colitis? Looking for a support group?




