Guillain-Barre Syndrome, also referred to as GBS, can cause paralysis of multiple parts of the body, along with incredible weakness and pain. Often referred to as GBS, the cause of this disorder is unknown, but it’s believed that a trigger related to surgery or illness exists. But what is Guillain-Barre Syndrome, exactly, and how does this autoimmune disorder progress?
What is Guillain-Barre Syndrome?
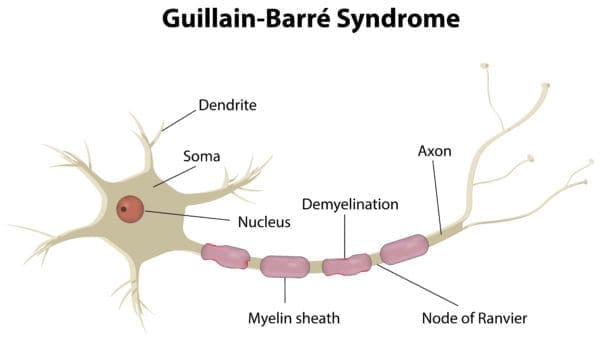
This rare disorder causes a person’s immune system to attack and damage their peripheral nervous system. The disorder attacks the myelin sheath, which is a fatty layer surrounding the nerves. As the myelin sheath is damaged, it can cause serious problems that affect how the nerves deliver signals to the brain and spinal cord. The nerve damage can slow down or stop the signals entirely, leading to paralysis, weakness, and pain.
According to the Centers for Disease Control and Prevention, approximately 3,000 to 6,000 people develop GSB annually. The syndrome affects both children and adults.
Guillain Barre Syndrome onset and symptoms
Most stories of people with GBS begin the same way: the condition’s quick onset can lead to paralysis in mere days or weeks. It usually strikes without warning and develops quickly, and about half of cases begin after a viral or bacterial infection, which can be as common as food poisoning or the flu. Some scientists believe that the infection prompts an autoimmune trigger, causing the patient’s antibodies and white blood cells to attack the myelin sheath of the nerves.
This rare disorder is so uncommon that many hospitals are not fully equipped to give a proper diagnosis. Sufferers are often sent home initially with a diagnosis of acute pain or idiopathic neuropathy, or they are referred to a neurologist for further investigation. Because this syndrome is a rare occurrence, it is important that patients advocate for themselves and be persistent when they know that something is not right with their bodies.
Symptoms could include:
- Tingling or numbness in the fingers and toes
- Muscle pain
- Loss of reflexes
- Low blood pressure
- Weakness or paralysis of partial or full body (difficulty walking)
- Paralysis that ascends up the limbs from the fingers and toes, moving in toward the torso
- Blurred vision
- Muscle contractions
- Respiratory difficulty or failure caused by paralysis
- Cardiovascular irregularity or dysfunction
- Difficulty swallowing and eating
- Fainting
- Drooling
Diagnosis
A GBS diagnosis can usually be confirmed within a number of tests. An ECG, EMG and nerve conduction velocity test are typically ordered to test muscle, nerve and brain function. After these tests, if the doctor is still suspicious, a spinal tap might be administered to look for elevated fluid protein in order to confirm the diagnosis.
If GBS is confirmed, treatment will begin immediately. Artificial breathing support may be administered. In the event of weakness to the muscles of the throat and chest, a feeding tube may be necessary.
Treatment options
There are also treatments that block the anti-bodies that attack the nerve cells. Plasma exchange treatments remove the blood from the body, separate the white and red blood cells, and return the anti-body-free blood cells back into the body. If this method doesn’t produce the desired results, doctors may try IVIG, or intravenous immunoglobulin therapy, a process that adds immunoglobulins to the blood in large-quantities, to aide in blocking anti-bodies. Blood-thinners, anti-inflammatories and narcotics may also be used to treat GBS as well.
Following these treatments, patients may need to participate in physical therapy. It is common for the disorder to disable a patient to the point that they might need to regain the ability to walk, or even relearn something as elementary as how to pick up a spoon.
Recovery
The recovery process can take months or years, but in most cases, people recover completely. While there is a likelihood that symptoms can be chronic and recurring, such symptoms are usually only minor neurological conditions, blood disorders, or weakness, and are much milder than paralysis or organ failure. Fatigue, pain, and muscle weaknesses aggravated by mild activity can be long-term symptoms that continue on after treatment.
It is possible, however, to develop more permanent symptoms if treatments are not administered immediately or are not aggressive enough. While such cases are rare, they are possible and should be considered.
Complications
Possible complications of Guillian-Barre Syndrome include:
- Pnuemonia or other respiratory conditions
- Blood clots
- Skin ulcers or damage
- Infections
- Permanent paralysis
- Heart conditions
It is important to also consider that unrelated ailments can become prevalent as a result of symptoms in their most severe state. Reports exist of GBS leading to respiratory failure, causing brain damage and epilepsy in some patients. Since the immune system is weak following treatment, there is also an increased risk for the development of other auto-immune disorders and viral infections. And, if joints become damaged, some patients may even develop irreparable, physical deformities.
How to move forward
It is important to immediately seek medical attention if you ever notice any significant changes in balance, coordination, or in your ability to walk and/or move your head and limbs. Experiencing pain, tingling or numbness in your extremities can also signify a serious medical condition, and these symptoms need to be addressed immediately.
The earlier GBS is caught, the milder the symptoms, the quicker the recovery and the greater the chance of a full recovery. Relapses are extremely rare, present in less than 10 percent of all cases. GBS is not genetic or contagious, although its exact origins and causes are unknown. Most GBS survivors recover with the ability to live happy and productive lives and without lingering complications that are severe enough to prevent working or raising a family.
Many support groups exist to help sufferers manage the disease and to offer a wide-range of resources and emotional support. For more information about Guillain-Barre Syndrome, research, and support, visit the Guillain-Barre Syndrome Foundation International.
What questions do you still have about Guillain-Barre Syndrome?
Ask us in the comments below.
What topics related to Guillain-Barre Syndrome would you like to see us explore?
Email us at info@painresource.com with your ideas!
Are you on Facebook?
Join our online community by clicking here.
This post was updated in January 2019 with new information and resources.



I had GBS in February of 2018. I had IVIG and then Plasma Exchange. I learned to walk again and am doing well for the most part. My right foot is numb and the first three toes on my right foot as well. I still have back pain after certain activities and wrist and thumb pain. I am wondering what the damaged nerves look like and if there is anything that can be done to repair them.
I had gbs one year ago and still have severe foot nerve pain when I walk for more than an hour or two. Is there anything I can take to lessen this pain.?