A team of scientists from Waterloo University’s Laboratory for Drug Delivery and Biomaterials and the University of Manitoba’s College of Pharmacy has recently developed a new “smart” device that can deliver two medications simultaneously, potentially stopping the transmission of human immunodeficiency virus (HIV).
The new device is an intravaginal ring, sometimes called an IVR, that can be inserted into the female genital tract, where it can then administer two medications that are known to decrease the transmission of HIV. Those medications include hydroxychloroquine (HCQ), an FDA-approved medication that is used for a wide array of autoimmune disorders, and a gene therapy nano medication that had been developed by the same group in previous studies.
“Before, only one drug could be delivered from an intravaginal ring.”
“We’ve specifically engineered a combination IVR that can deliver two unique medications targeting different aspects of the HIV infection process,” said Emmanuel Ho, an associate professor at the University of Waterloo’s School of Pharmacy and the study’s corresponding author, adding, “Before, only one drug could be delivered from an intravaginal ring.”
Typically, the most effective method of preventing the spread of HIV is through the use of condoms. However, researchers involved with the study say their new device could be useful for sex workers or in situations in which women are not in a position to negotiate condom use.
The ring is made of two segments of medical-grade plastic and is just two centimeters (.79 inches) in diameter—no larger than a US penny. One half of the ring is solid and coated with a pH-sensitive material that releases the team’s gene therapy treatment. The other half is hollow and has tiny perforations to allow the HCQ to be released slowly over 25 days.
The truly “smart” aspect of the ring is its ability to release its drugs specifically during intercourse. The solid half of the ring, coated in a pH-sensitive polymer, reacts in the presence of semen, which allows it to release the nanomedicine only during intercourse.
“We are hoping that this will reduce the cost of drug therapy and also prevent users from developing drug resistance.”
“This IVR system will help women to protect themselves against HIV infection and greatly reduce drug usage when it is not necessary,” says Yannick Traore, a recent Waterloo Ph.D. graduate and lead author on the study.”We are hoping that this will reduce the cost of drug therapy and also prevent users from developing drug resistance.”
In the team’s laboratory tests, the ring proved to be extremely successful. Upon testing, the ring was able to successfully release its HCQ over 25 days, and the pH-sensitive half was able to accurately detect and respond to the presence of seminal fluid. When exposed to an artificially created seminal fluid the ring’s “smart” half was able to release 20 times more of its gene therapy medication than when only exposed to vaginal fluids.
The group says its next steps are to move on to animal trials, where they will gain a greater understanding of how the ring would function in a more real-world scenario.
What Questions About the “Smart” Ring Do You Have?
Ask away in the comments section below!
What Topics Should We Cover Next?
Email us at info@painresource.com with your ideas.
Are you on Facebook?

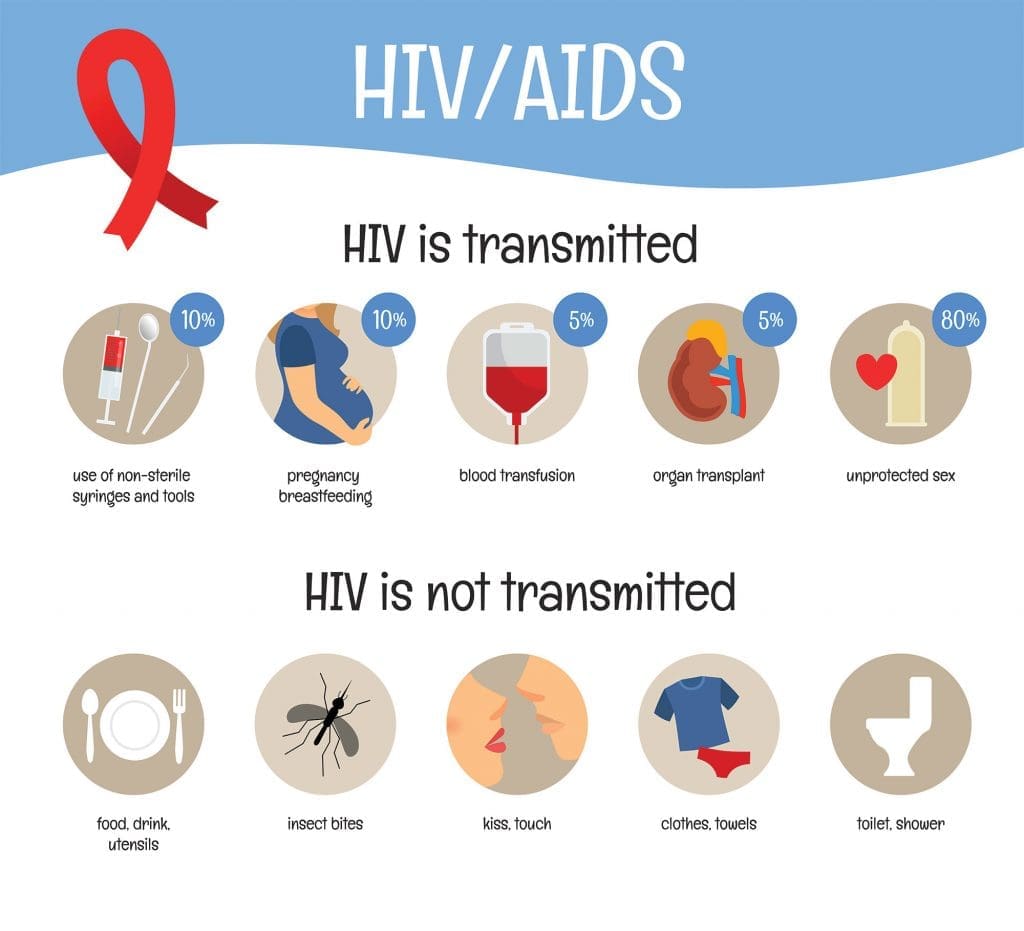




The first row of the infographic implies transmission routes total 110%. True, there could be some overlap, but surely not that much, eh?)