Tammy Wynette sure knew what she was talking about back in 1969—sometimes it is hard to be a woman. Especially when it comes to pelvic pain. Men experience pelvic pain, too, but it’s far more common in women. In this article, I’ll cover common causes of pelvic pain in women, treatment options, and when it’s time to see a doctor.
What Is Pelvic Pain?
Pelvic pain is pain in the lower abdomen and pelvis area. It can be sharp and stabbing or a dull, aching sensation. Some pelvic pain is acute—short-term but sudden and severe. Or it can be chronic—the pain comes and goes or is constant. Because there are many organs in the lower abdominal area, chronic pelvic pain can be hard to diagnose and treat.
Acute Pelvic Pain
Underlying illness can cause acute pelvic pain. But in women, it’s more commonly related to the reproductive system. Here are some common causes of acute pelvic pain:
 Gynecological Causes
Gynecological Causes
- Menstrual cramps.
- Mittelschmerz: Many women can feel pain in the pelvic area midway through their cycle when they ovulate.
- Ectopic pregnancy. A pregnancy outside the uterus (usually a fallopian tube).
- Sexually-transmitted disease (STD). Chlamydia and gonorrhea are the most common.
- Miscarriage.
Other Causes
- Urinary tract infection (UTI): An infection anywhere in the urinary system.
- Constipation: Can cause pain in the pelvis or lower back.
- Digestive problems.
Chronic Pelvic Pain
Common causes of chronic pelvic pain include:
Gynecological Causes
- Pelvic inflammatory disease. An infection that’s usually (but not always) caused by an STD.
- Ovarian cyst. A fluid-filled sac in an ovary. This happens during ovulation. An egg travels through a fallopian tube to the follicles on the end, but the follicle does not release the egg as usual. Most ovarian cysts are harmless and disappear on their own in one to three months.
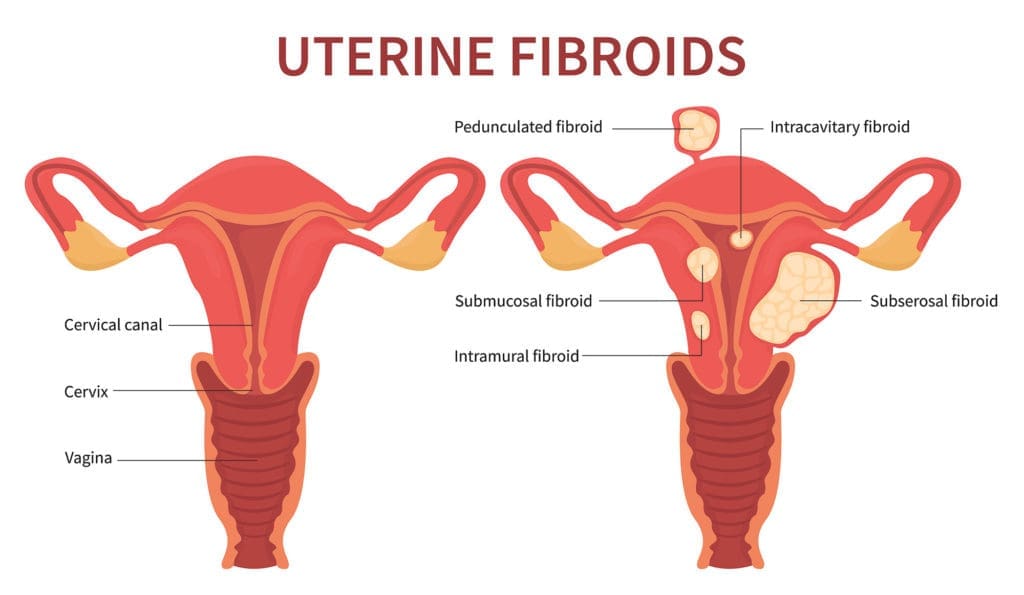
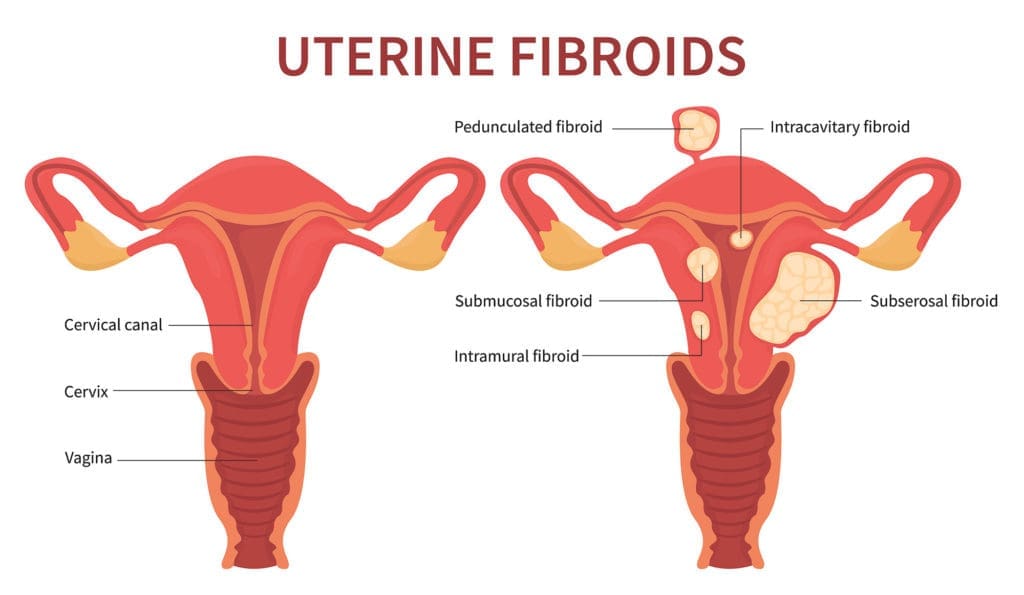
- Uterine fibroids. Tumors in the uterus. They are usually harmless but can cause pain.
- Endometriosis. The tissue lining the uterus grows outside the uterus. Endometriosis can cause excruciating pain.
- Adhesions. Scar tissue caused by endometriosis, inflammation, infection, or surgery.
Other Causes
- Irritable bowel syndrome. Long-term abdominal pain with changes in bowel habits, sometimes alternating between constipation and diarrhea. The pain is often worse after meals. There’s usually no known cause.
- Urinary tract infection.
- Kidney stones.
- Digestive disorders such as Crohn’s disease.
- Interstitial cystitis: Pain in the bladder for more than six weeks.
- Pelvic organ prolapse: Muscle weakness causes the bladder or uterus to drop and protrude into, or even out of, the vagina.
- Pelvic congestion syndrome: Blood builds up in veins in the abdomen. The veins enlarge and lose their shape, like varicose veins in the legs.
- Adhesions (see above).
- Pain with sexual activity (dyspareunia).
Treatment for Chronic Pelvic Pain
Surgery
Exploratory laparoscopy: When women have pelvic pain without an apparent cause, and nothing shows on a CT scan, your doctor may recommend an exploratory laparoscopy. They will insert a thin tube with a tiny camera on the end through a small incision in your abdomen. They will then look for anything that’s not normal. According to a 2018 review study, surgeons performed 40% of exploratory laparoscopies for chronic pelvic pain in women. In 98% of those cases, they found something wrong. In 75% of cases, they found a diagnosis. And 59% of patients said their pain was improved afterward.
Hysterectomy: In rare and severe cases, doctors may suggest hysterectomy—removing the uterus—with or without ovaries and fallopian tubes.
Medication
Because many women with CPP never find the cause of their pain, doctors usually focus on treating symptoms. The process is sometimes based on trial and error. The most common medications for CPP, according to Mayo Clinic, include:
Pain relievers: Doctors usually suggest over-the-counter pain medications like Tylenol or ibuprofen. In severe cases, they may recommend prescription pain medication. However, pain medication rarely solves the problem that’s causing the pain.
Hormone treatment: For pain that’s related to the menstrual cycle, hormone treatment may help. Doctors sometimes prescribe birth control pills, for example, or other hormonal medicines.
Antibiotics: Providers may prescribe antibiotics if an infection is the cause of the pain.
Antidepressants: Some antidepressants can treat pain as well as depression. Doctors may prescribe these even for women who don’t have depression.
Integrative Therapy


- Pelvic floor physical therapy.
- Psychotherapy.
- Yoga.
- Massage.
- Biofeedback.
- Acupuncture.
- Nerve stimulation therapy.
- Dry needling.
- Herbal remedies.
- Meditation.
- Cognitive-behavioral therapy.
- Relaxation techniques.
- Support groups.
These alternative therapies are often called complementary because providers use them to complement, or work alongside, traditional treatments. If you’re interested in exploring complementary therapies, ask your provider for recommendations. You could also call a local hospital to find out what’s available in your area.
When to See a Doctor for Pelvic Pain
When a person is in pain most of the time, it can be hard to know when to call the doctor. Use the following as your guide. Call your provider if:
- You have new pain or sudden pain that’s worse than usual.
- Your typical pain is worsening.
- You have menstrual pain after your period is over.
- You have symptoms to suggest pelvic inflammatory disease or ectopic pregnancy.
- Your pain is interfering with your daily activities.
A Final Word on Pelvic Pain
If you suffer from chronic pain, it’s hard not to feel hopeless sometimes. But researchers are working on it and finding new ways to treat pain. With good self-care and knowing when to ask for help, you can find ways to deal with your pelvic pain and reclaim your life.
How do you deal with pelvic pain?
Comment below to share your story
What pelvic pain issues do you want to learn more about?
Email us at info@painresource.com with your ideas!
Are you on Facebook?
Join our online community by clicking here.




