What Is Chronic Pain and Why Is It Important?
Chronic pain is pain that lasts more than several months (variously defined as 3 to 6 months, but certainly longer than “normal healing”). It’s a very common problem. Results from the 2012 National Health Interview Survey show that:
- About 25.3 million U.S. adults (11.2 percent) had pain every day for the previous 3 months.
- Nearly 40 million adults (17.6 percent) had severe pain.
- Individuals with severe pain had worse health, used more health care, and had more disability than those with less severe pain.
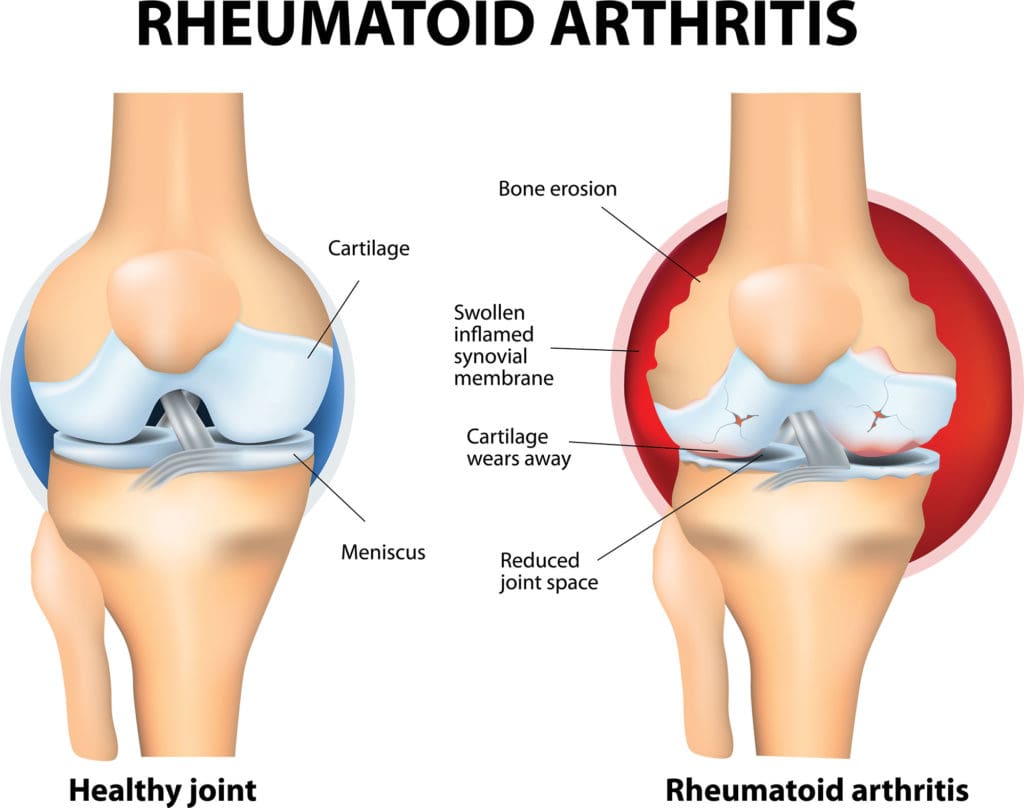
 Chronic pain becomes more common as people grow older, at least in part because health problems that can cause pain, such as osteoarthritis, become more common with advancing age. Not all people with chronic pain have a physician-diagnosed health problem, but among those who do, the most frequent conditions by far are low-back pain or osteoarthritis, according to a national survey. Other common diagnoses include rheumatoid arthritis, migraine, carpal tunnel syndrome, and fibromyalgia. The annual economic cost of chronic pain in the United States, including both treatment and lost productivity, has been estimated at nearly $635 billion.
Chronic pain becomes more common as people grow older, at least in part because health problems that can cause pain, such as osteoarthritis, become more common with advancing age. Not all people with chronic pain have a physician-diagnosed health problem, but among those who do, the most frequent conditions by far are low-back pain or osteoarthritis, according to a national survey. Other common diagnoses include rheumatoid arthritis, migraine, carpal tunnel syndrome, and fibromyalgia. The annual economic cost of chronic pain in the United States, including both treatment and lost productivity, has been estimated at nearly $635 billion.
Chronic pain may result from an underlying disease or health condition, an injury, medical treatment (such as surgery), inflammation, or a problem in the nervous system (in which case it is called “neuropathic pain”), or the cause may be unknown. Pain can affect quality of life and productivity, and it may be accompanied by difficulty in moving around, disturbed sleep, anxiety, depression, and other problems.1
For more information about chronic pain, visit the National Institute of Neurological Disorders and Stroke.
What the Science Says About Complementary Health Approaches for Chronic Pain
The scientific evidence suggests that some complementary health approaches may help people manage chronic pain.
A comprehensive description of scientific research on all the complementary approaches that have been studied for chronic pain is beyond the scope of this fact sheet. This section highlights the research status of some approaches used for common kinds of pain.
Chronic pain in general
Some recent research has looked at the effects of complementary approaches on chronic pain in general rather than on specific painful conditions.
- A 2014 evaluation of studies on active self-care complementary approaches (approaches that individuals can do themselves after being taught the technique) found that there is some evidence in favor of using yoga, tai chi, and music for self-management of chronic pain symptoms, but not enough to justify a strong recommendation for their use. The evidence is insufficient, according to this evaluation, to allow conclusions to be reached about other self-care approaches such as mindfulness/meditation, relaxation techniques, and qi gong.
- A 2016 evaluation of the research on mindfulness-based interventions found they may be helpful for patients with chronic pain, with effectiveness similar to that of cognitive-behavioral approaches.
- Research shows that hypnosis is moderately effective in managing chronic pain, when compared to usual medical care. However, the effectiveness of hypnosis can vary substantially from one person to another.
- There’s some evidence that cannabinoids (substances from marijuana) might be helpful for chronic neuropathic or cancer pain.
Low-back pain


- A 2012 combined analysis of data from several studies concludes that acupuncture is a reasonable option to consider for chronic low-back pain. How acupuncture works to relieve pain is unclear. Current evidence suggests other factors—like expectation and belief—that are unrelated to acupuncture needling may play important roles in the beneficial effects of acupuncture on pain. A 2016 review of studies conducted in the United States found evidence that acupuncture can help some patients manage low-back pain.
- Massage might provide short-term relief from low-back pain, but the evidence is not of high quality. Massage has not been shown to have long-term benefits on low-back pain.
- There is some evidence that progressive relaxation may help relieve low-back pain, but studies on this topic have not been of the highest quality.
- Spinal manipulation appears to be as effective as other therapies commonly used for chronic low-back pain, such as physical therapy, exercise, and standard medical care.
- Studies have shown that yoga can be helpful for low-back pain in the short term and may also be helpful over longer periods of time.
- A 2014 evaluation of research on herbal products for low-back pain found preliminary evidence that devil’s claw and white willow bark, taken orally (by mouth), may be helpful for back pain. Cayenne, comfrey, Brazilian arnica, and lavender essential oilmay be helpful when used topically (applied to the skin).
- Studies of prolotherapy (a treatment involving repeated injections of irritant solutions) for low-back pain have had inconsistent results.
Osteoarthritis
- A 2012 combined analysis of data from several studies indicated that acupuncture can be helpful and a reasonable option to consider for osteoarthritis pain. After that analysis was completed, a 2014 Australian study showed that both needle and laser acupuncture were modestly better than no treatment at relieving knee pain from osteoarthritis but not better than simulated (sham) laser acupuncture. These results generally agree with previous studies, which showed that acupuncture is consistently better than no treatment but not necessarily better than simulated acupuncture at relieving osteoarthritis pain.
- A small amount of research suggests that massage may help reduce osteoarthritis symptoms.
- Tai chi may improve pain in people with knee osteoarthritis. Qi gong may have similar benefits, but little research has been done on it.
- It’s uncertain whether yoga is helpful for osteoarthritis.
- Studies of glucosamine, chondroitin, and S-adenosyl-L-methionine (SAMe) for knee osteoarthritis pain have had conflicting results.
- There isn’t enough research on dimethyl sulfoxide (DMSO) or methylsulfonylmethane (MSM) for osteoarthritis pain to allow conclusions to be reached.
More information on complementary health approaches for osteoarthritis
Rheumatoid Arthritis
- The amount of research on mind and body practices for rheumatoid arthritis pain is too small for conclusions to be reached about their effectiveness.
- Dietary supplements containing omega-3 fatty acids, gamma-linolenic acid (GLA), or the herb thunder god vine may help relieve rheumatoid arthritis symptoms.
More information on complementary health approaches for rheumatoid arthritis
Headache
- A 2012 combined analysis of data from several studies indicates that acupuncture can be helpful and a reasonable option to consider for headache pain. How acupuncture works to relieve pain is unclear. Current evidence suggests that many factors—like expectation and belief—that are unrelated to acupuncture needling may play important roles in the beneficial effects of acupuncture on pain.
- Because the evidence is limited or inconsistent, it’s uncertain whether biofeedback, massage, relaxation techniques, spinal manipulation, and tai chi are helpful for headaches.
- Guidelines from the American Academy of Neurology and the American Headache Society classify butterbur as effective; feverfew, magnesium, and riboflavin as probably effective; and coenzyme Q10 as possibly effective for preventing migraines.
More information on complementary health approaches for headache
Neck Pain
- Acupuncture hasn’t been studied as extensively for neck pain as for some other conditions. A large study in Germany found that people who received acupuncture for neck pain had better pain relief than those who didn’t receive acupuncture. Several studies have compared actual acupuncture with simulated acupuncture, but the amount of research is limited. No current guidelines recommend acupuncture for neck pain.
- A 2016 review of studies performed in the United States found that massage therapymay provide short-term relief from neck pain, especially if massage sessions are relatively lengthy and frequent.
- Spinal manipulation may be helpful for neck pain.
Fibromyalgia
- It’s uncertain whether acupuncture is helpful for fibromyalgia pain.
- Although some studies of tai chi, yoga, mindfulness, and biofeedback for fibromyalgia symptoms have had promising results, the evidence is too limited to allow definite conclusions to be reached about whether these approaches are helpful.
- There is insufficient evidence that any natural products can relieve fibromyalgia pain, with the possible exception of vitamin D supplements, which may reduce pain in people with fibromyalgia who have low vitamin D levels.
- Studies of homeopathy have not demonstrated that it is beneficial for fibromyalgia.
Irritable bowel syndrome


- Although no complementary health approach has definitively been shown to be helpful for irritable bowel syndrome, some research results for hypnotherapy and probioticshave been promising.
- There’s only weak evidence supporting the idea that peppermint oil might be helpful for irritable bowel symptoms.
- Studies of acupuncture for irritable bowel syndrome have not found actual acupuncture to be more helpful than simulated acupuncture.
More information on complementary health approaches for irritable bowel syndrome
Other types of pain
- Various complementary approaches have been studied for other types of chronic pain, such as facial pain, nerve pain, chronic pelvic pain, elbow pain, pain associated with endometriosis, carpal tunnel syndrome, pain associated with gout, and cancer pain. There’s promising evidence that some complementary approaches may be helpful for some of these types of pain, but the evidence is insufficient to clearly establish their effectiveness.
Other complementary approaches
- There is a lack of high-quality research to definitively evaluate whether Reiki is of value for pain relief.
- Although static magnets are widely marketed for pain control, the evidence does not support their use.
What the Science Says About Safety and Side Effects
As with any treatment, it’s important to consider safety before using complementary health approaches. Safety depends on the specific approach and on the health of the person using it. If you’re considering or using a complementary approach for pain, check with your health care providers to make sure it’s safe for you.
Safety of Mind and Body Approaches
- Mind and body approaches, such as acupuncture, hypnosis, massage therapy, mindfulness/meditation, relaxation techniques, spinal manipulation, tai chi/qi gong, and yoga, are generally safe for healthy people if they’re performed appropriately.
- People with medical conditions and pregnant women may need to modify or avoid some mind and body practices.
- Like other forms of exercise, mind and body practices that involve movement, such as tai chi and yoga, can cause sore muscles and may involve some risk of injury.
- It’s important for practitioners and teachers of mind and body practices to be properly qualified and to follow appropriate safety precautions.
- See the Health Topics A–Z list on the NCCIH Web site for resources about specific mind and body practices, including information about their safety.
Safety of Natural Products
For more information on complementary health approaches that have been studied for pain, see:
Guidelines for the Treatment of Chronic Pain Conditions
The American College of Rheumatology mentions several complementary approaches in its guidelines for the management of osteoarthritis of the hip or knee. For osteoarthritis of the knee, the guidelines mention tai chi as one of several nondrug approaches that might be helpful. The same guidelines, however, discourage using the dietary supplements glucosamine and chondroitin for osteoarthritis of the hip or knee.
The American College of Gastroenterology (ACG) included probiotics/prebiotics, peppermint oil, and hypnotherapy in its evaluation of approaches for managing irritable bowel syndrome. The ACG found only weak evidence that any of these approaches may be helpful.
For more information, see the Health Professional Information section of NCCIH’s Web page on Pain.
NCCIH-Funded Research
NCCIH is part of the National Institutes of Health (NIH) Pain Consortium, which coordinates pain research across NIH. NCCIH-supported studies are helping to build an evidence base on the effectiveness and safety of complementary modalities for treating chronic pain.
More about NCCIH-funded pain research
In addition, NCCIH’s Division of Intramural Research conducts research focusing on the role of the brain in perceiving, modifying, and managing pain. Research projects include investigating the role of the brain in pain processing and control, and how factors such as emotion, attention, environment, and genetics affect pain perception.
In light of the human and economic costs of chronic pain, as well as evidence that many people who have chronic pain turn to complementary health approaches for relief, NCCIH places a high priority on pain-related research. Researchers in this area face unique challenges: much remains to be understood about the nature of chronic pain and about the best ways of studying its many causes, people’s different responses, and the value of various treatment approaches—complementary and conventional. The ultimate goal is to build an evidence base that can guide pain management decisions tailored to individuals. These decisions often involve combining treatment approaches in cost-effective ways that do the best possible job of helping people minimize pain, carry out everyday activities, and improve their quality of life.
While building an evidence base to help people with chronic pain and their health care providers make decisions about pain management, research on complementary health approaches is also helping to close gaps in our basic understanding of pain mechanisms.
If You Are Considering Complementary Health Approaches for Chronic Pain
- Do not use an unproven product or practice to replace conventional care or to postpone seeing a health care provider about chronic pain or any other health problem.
- Learn about the product or practice you are considering, especially the scientific evidence on its safety and whether it works.
- Talk with the health care providers you see for chronic pain. Tell them about the product or practice you are considering and ask any questions you may have. They may be able to advise you on its safety, use, and likely effectiveness.
- If you are considering a practitioner-provided complementary health practice such as spinal manipulation, massage, or acupuncture, ask a trusted source (such as your health care provider or a nearby hospital) to recommend a practitioner. Find out about the training and experience of any practitioner you are considering. Ask whether the practitioner has experience working with your pain condition.
- If you are considering dietary supplements, keep in mind that they can cause health problems if not used correctly, and some may interact with prescription or nonprescription medications or other dietary supplements you take. Your health care provider can advise you. If you are pregnant or nursing a child, or if you are considering giving a child a dietary supplement, it is especially important to consult your (or your child’s) health care provider. To learn more, visit NCCIH’s Web page on dietary supplements.
- Tell all your health care providers about any complementary or integrative health approaches you use. Give them a full picture of what you do to manage your health. This will help ensure coordinated and safe care.
1 Certain chronic conditions, several of which cause pain, may occur together; some individuals have two or more of these problems. These conditions include chronic fatigue syndrome, endometriosis, fibromyalgia, interstitial cystitis (painful bladder syndrome), irritable bowel syndrome, temporomandibular joint dysfunction, and vulvodynia (chronic vulvar pain). It is not known whether these disorders share a common cause.
What’s the Bottom Line?
How much do we know about the effectiveness of complementary health approaches for chronic pain?
- A growing body of evidence suggests that some complementary approaches, such as acupuncture, hypnosis, massage, spinal manipulation, and yoga, may help to manage some painful conditions.
What do we know about the safety of complementary health approaches for chronic pain?
- Although many of the complementary approaches studied for chronic pain have good safety records, that doesn’t mean that they’re risk-free for everyone. Your health, special circumstances (such as pregnancy), and medicines or supplements that you take may affect the safety of complementary approaches.
For More Information
NCCIH Clearinghouse
The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature. The Clearinghouse does not provide medical advice, treatment recommendations, or referrals to practitioners.
Toll-free in the U.S.: 1-888-644-6226
TTY (for deaf and hard-of-hearing callers): 1-866-464-3615
Web site: nccih.nih.gov
E-mail: info@nccih.nih.gov(link sends e-mail)
National Institute of Neurological Disorders and Stroke (NINDS)
NINDS conducts and supports research on how the brain and nervous system function and on treatments for neurological diseases.
Toll-free in the U.S.: 1-800-352-9424
Web site: www.ninds.nih.gov
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS)
The mission of NIAMS is to support research into the causes, treatment, and prevention of arthritis and musculoskeletal and skin diseases; the training of basic and clinical scientists to carry out this research; and the dissemination of information on research progress in these diseases.
Toll-free in the U.S.: 1-877-22-NIAMS
Web site: www.niams.nih.gov
PubMed®
A service of the National Library of Medicine, PubMed® contains publication information and (in most cases) brief summaries of articles from scientific and medical journals. For guidance from NCCIH on using PubMed, see How To Find Information About Complementary Health Approaches on PubMed.
Web site: www.ncbi.nlm.nih.gov/pubmed
Cochrane Database of Systematic Reviews
The Cochrane Database of Systematic Reviews is a collection of evidence-based reviews produced by the Cochrane Library, an international nonprofit organization. The reviews summarize the results of clinical trials on health care interventions. Summaries are free; full-text reviews are by subscription only.
Web site: www.cochranelibrary.com
NIH Clinical Research Trials and You
The National Institutes of Health (NIH) has created a Web site, NIH Clinical Research Trials and You, to help people learn about clinical trials, why they matter, and how to participate. The site includes questions and answers about clinical trials, guidance on how to find clinical trials through ClinicalTrials.gov and other resources, and stories about the personal experiences of clinical trial participants. Clinical trials are necessary to find better ways to prevent, diagnose, and treat diseases.
Web site: www.nih.gov/health/clinicaltrials/
MedlinePlus
To provide resources that help answer health questions, MedlinePlus (a service of the National Library of Medicine) brings together authoritative information from the National Institutes of Health as well as other Government agencies and health-related organizations.
Web site: www.medlineplus.gov
Key References
- Crawford C, Lee C, Buckenmaier C III, et al. The current state of the science for active self-care complementary and integrative medicine therapies in the management of chronic pain symptoms: lessons learned, directions for the future. Pain Medicine. 2014;15 (suppl 1):S104-S113.
- Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. American Journal of Gastroenterology. 2014;109 (suppl 1):S2-S26.
- Furlan AD, Giraldo M, Baskwill A, et al. Massage for low-back pain. Cochrane Database of Systematic Reviews. 2015;(9):CD001929. Accessed at www.cochranelibrary.com on November 11, 2015.
- Gross A, Langevin P, Burnie SJ, et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database of Systematic Reviews. 2015;(9):CD004249. Accessed at www.cochranelibrary.com on November 11, 2015.
- Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care & Research. 2012;64(4):465-474.
- Holland S, Silberstein SD, Freitag F, et al. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults. Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1346-1353.
- Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. The National Academies Press Web site. Accessed at http://www.nap.edu/catalog.php?record_id=13172 on March 7, 2016.
- Manheimer E, Cheng K, Wieland LS, et al. Acupuncture for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews. 2012;(5):CD005111. Accessed at www.cochranelibrary.com on March 11, 2016.
- Nahin RL, Boineau R, Khalsa PS, Stussman BJ, Weber WJ. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clinic Proceedings. 2016;91(9):1292-1306.
- Nahin RL. Estimates of pain prevalence and severity in adults: United States. 2012. Journal of Pain. 2015;16(8);769-780.
- Rubinstein SM, van Middelkoop M, Assendelft WJ, et al. Spinal manipulative therapy for chronic low-back pain. Cochrane Database of Systematic Reviews. 2011;(2):CD008112 [edited 2013]. Accessed at www.cochranelibrary.com on March 8, 2016.
- Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Archives of Internal Medicine. 2012;172(19):1444-1453.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
All Other References
Acknowledgments
NCCIH thanks Partap Khalsa, D.C., Ph.D., and David Shurtleff, Ph.D., NCCIH, for their contributions to the 2016 update of this publication.
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your primary health care provider. We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your primary health care provider. We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.
Source: NIH
What subjects on chronic pain would you like more information on?
Let us know by emailing us at info@painresource.com or sharing your thoughts in the comments below.
Are you on Facebook?
Join our online community by clicking here