At the age of 21, I was diagnosed with multiple spine and pelvis disorders which flipped my life upside down. Health professionals label me as the “21-year-old with a 90-year-old spine”. The main cause of my declining spine? Degenerative disc disease.
What is Degenerative Disc Disease?
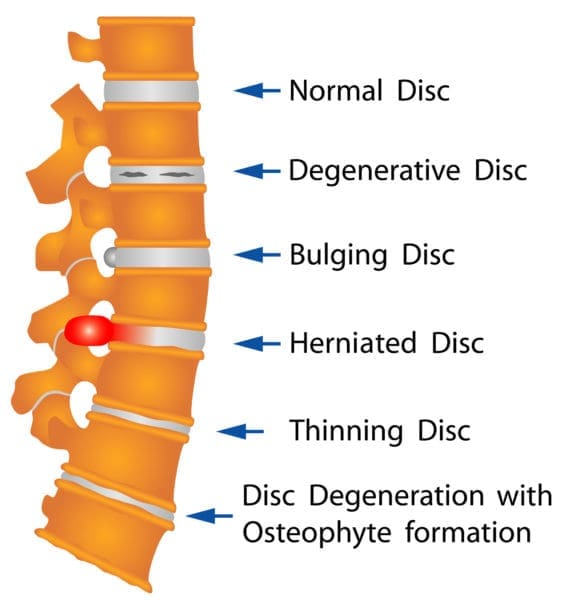
Believe it or not, degenerative disc disease (DDD) isn’t classified as an actual disease. Instead, it’s a progressive condition attributed to the normal process of aging. Whether it’s due to strain, overuse or incorrect use, the intervertebral discs in your spine degenerate as you age. However, in some people, it can occur more rapidly due to underlying diseases or injuries to the spine.
The intervertebral discs cushion the space between the bony vertebrae in your spine. These spinal discs act as shock absorbers, helping your body stay flexible, stand up straight, twist and bend over. As we age, these discs lose moisture, resulting in decreased shock absorption and increased risk of wear and tear. The discs can then begin to lose their height, bringing the vertebrae closer together, which leads to spinal canal narrowing, restricted movement, break down of cartilage, pain and spinal nerve compression.
Causes
The main cause of degenerative disc disease is aging. However, multiple risk factors can speed up the process of disc degeneration and cause it to occur at a young age. If someone gets DDD at a younger age, it’s usually because of:
- acute or sudden injury (such as a fall)
- genetics
- pre-existing prematurely aging spine
- obesity
- physical work that strains the back
- smoking
- conditions affecting the biomechanics of the spine (such as scoliosis and arthritis)
Symptoms
The bones of the spine are made up of four sections, each consisting of a certain number of vertebrae. Each level in the spine has a series of spinal nerves that are connected to various organs and body parts. Depending on what part of the spine degenerates, different symptoms can appear. Some of the most common symptoms of degenerative disc disease include:
- mild, severe, or debilitating discomfort
- pain, weakness, and discomfort in the back that radiates to another area
- tingling and/or numbness in the legs or feet
- instability in the spine, leading to muscle spasms in the lower back or neck as the body tries to correct and stabilize
- flareups of intense pain
- pain that worsens when sitting, bending, lifting and twisting
- difficulty walking
- weakness in leg muscles or a foot drop (indicates that there may be damage to the nerve root)
Diagnosis
It’s important to get a diagnosis from a healthcare professional as soon as you notice any symptoms. You doctor will get a brief history and ask about the details of your pain. You may also undergo some physical tests including, but not limited to:
- palpation
- reflex tests
- muscle strength
- flexibility
- motion tests
Sometimes, your doctor may also send you for imaging to identify any abnormalities including:
- MRI scans
- CT scans
- bone scans
- X-rays
Treatment
The aim of treatment is to reduce the baseline chronic pain levels and prevent flareups as much as possible. Treatments can vary depending on the severity of the symptoms and how much they limit your daily activities. It is highly likely that even though the discs in your spine will continue to age, your back pain will decrease as the symptoms become more manageable. The most important part of preventing DDD is to get your pain under control, increase the strength and flexibility in the muscles that surround and support the spine, and improve mobility.


Most patients do not require surgery and their pain can be managed with the following treatments:
- Medications, including NSAIDs (OTC and prescription)
- Physical Therapy (back and neck exercises, stretching, strengthening exercises, hydrotherapy, etc. to decrease pain, help improve movement and strength, and painful swelling)
- Chiropractic care (manual manipulation to relieve muscle tension, remove pressure from nerve roots, and relieve tension in the joints)
- Steroid injections (to help decrease pain and inflammation around the discs)
- Clinical pilates
- Cold and hot packs (decreases pain, inflammation and muscle spasms)
- Tens device electrical stimulation (TENS – sends electrical pulses through the body that interfere with and minimize pain signals)
- Ergonomic furniture to support the spine (desk chairs, standing desks, neck pillows)
- Diet (drink water, increase your nutrients and minerals, increase protein for muscle growth, maintain a healthy weight)
- Adequate sleep, to let the body recover and relax
Unfortunately for more severe cases of DDD, surgical intervention may be required for pain relief. Possible surgeries include:
- Spinal Fusion
- Discectomy
- Laminectomy
Please note there are always several factors to consider before opting for surgery and make sure you speak with your doctor about this.
My Experience with DDD
Degenerative Disc Disease has changed my life in a lot of ways. My pain levels can change in a split second, and would sometimes leave me stuck in bed all day, unable to move due. I became unreliable as a friend and lost some of those close to me. I was unable to work, walk, exercise, shower or dress myself, or even brush my own hair. At the young age of 21, I lost my independence.


In December 2018, I had a discectomy after doctors found one of my degenerated discs bulged and wrapped around my spinal cord. Before the operation, I was practically disabled, but afterward, I was told I needed to push myself to get better. My surgeon told me that if I continued to stay bedridden, I would never recover. I tried to exercise as much as I could, but my body was so exhausted that I could barely keep up.
Because this condition will only progress as I age, I will have to deal with DDD for the rest of my life. However, now that I am 7 months post-op, I have gone back to using conservative treatments for my discomfort and pain. I am able to effectively manage my symptoms with hydrotherapy, walking programs, yoga, pain medication, a well-controlled diet, acupuncture, massage, and physiotherapy. Yoga and hydrotherapy have been a godsend! The low impact exercises relieve pressure off my joints and in turn, improve my symptoms.
Seeing a psychologist once a month has helped my mindset and attitude towards my pain. I have been able to return to work full time and now live a busy life. Occasionally, I lose the ability to walk or feel numb and weak, but only for short periods of time.
Conclusion
Degenerative disc disease is a natural part of the aging process, and the effect it has on your life and the pain levels and symptoms associated with it is different for everyone. Make sure you try non-surgical treatments first and get advice from your healthcare team to ensure its safe for you. Please contact your health care provider if you have any concerns or questions. Remember to stay healthy and active, take control of your health and make the steps necessary to look after your back and spine health!
Do you have a story about chronic pain you’d like to share?
What topics related to spine health and chronic pain would you like to see us explore?
Email us with your ideas!
Are you on Facebook?
Join our online community by clicking here.





I was in high school when I was diagnosed but the symptoms of a bulging disc was diagnosed now that I am 24.
Thank you for this article. It made me feel like I could learn to live with it, since other young people have also been diagnosed with it.
I was 45 when I was diagnosed with disc degenerative disease. I had woke up one morning and felt as if my neck became unhinged. It took me an hour to be able to get up and go to a doctor. After telling the doctor my symptoms he wanted to take an x-ray. The x-ray showed 3 herniated discs bulging into my spinal cord cutting off csf to my brain and in turn pressing my cord causing my right arm to atrophy. I thought that that issue was my shoulder. Boy was I wrong. The doctor suggested I see a specialist and get and MRI. The MRI showed I had cervical stenosis with severe myopathy. My canal was 6mm. C3-C7. After 8hrs surgery and a week in the hospital I now have a plate in front and 2 rods and 8pins in my neck. They removed and fused the damage. I have very limited movement in my neck. 3years have passed and I feel like it’s happening all over again. Weakness in my arm and slightly tingling fingers. Imbalanced walking. My neck constantly feels pulled and strained. Only now I’m feeling the grinding in my lower lumbar. If this disease is so progressive and irreversible I wonder about the quality of my life. Even more so now then ever.